Prematurity is the gift that keeps on giving.
Even if you were lucky enough to escape the NICU with no lingering complications, sometimes issues will crop up much later that leave you wondering if prematurity is rearing its ugly head again.
For us, it has been hearing issues. Is it related to prematurity, genetics, or the luck of the draw? No way to tell, though his early arrival did play into our decision to go the route of ear tubes. There is plenty of information out there about ear infections in kids, so I want to give you a rundown of what the actual process was like for us. Yours may be different in some ways but I bet a lot will be similar.
Initial Testing
Rowan was born at 31 weeks in late April 2015. He passed the newborn hearing screening in the NICU. When he was around six months adjusted, he had a bout of RSV, followed by his first ear infection. It is not clear whether he then had a series of several recurring infections or one long infection that took several antibiotics to clear up.
When he was just a bit past one year adjusted he had his first follow-up hearing test. I sat in a small booth with him on my lap and an audiologist sitting next to us. There was another audiologist on the other side of the sound-proof glass.
The first test was Tympanometry, or putting sensors in his ears that checked the flexibility of his eardrums. They were quite stiff, which the doctor said was likely due to fluid behind the drum.
Then the audiologist behind the glass called Rowan’s name and when he looked towards the sound he was rewarded with a clip of a cartoon or a spinning puppet. This conditioned him that looking towards the sound = reward. From that point, they played a series of different tones at varying volumes. There was one tone that he did not respond to, so they put a little bone conduction sensor behind his ear to ensure the problem was conductive, meaning it was an issue with the outer or middle ear. This was the case for Rowan.
Results & Diagnosis
We had a follow-up appointment three months later, with the same results. At this point, they referred us to an Ear, Nose, and Throat specialist (ENT). We had our appointment two months later, where his eardrums were still stiff.
Keep in mind that we had not had any more noticeable ear infections since the RSV almost a year prior, so tubes were not really on my radar. I incorrectly thought tubes were only indicated in the presence of repeated severe infections.
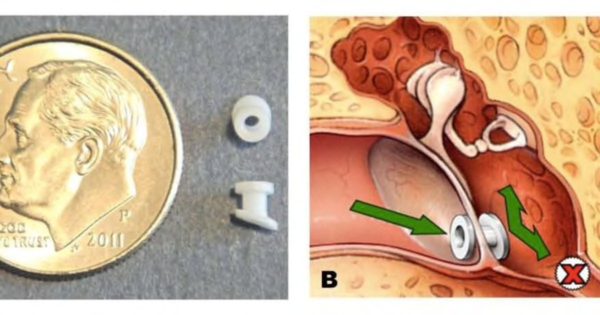
Photo: Rosenfeld RM. A Parent’s Guide to Ear Tubes. Hamilton: BC Decker Inc., 2005.
The doctor explained that sometimes, even without recurrent infection, the pressure in the ear does not equalize normally and there is chronic fluid behind the ear. That, coupled with his failed hearing tests, borderline speech development, and increased risk of developmental delays (hello, prematurity!), was enough for him to recommend tubes.
The tubes would allow his ears to drain and hopefully improve his hearing and possibly his comfort. So I said yes. The doctor then showed me one of the tubes and I was amazed by just how tiny it really is. Think, grain of rice.
He had a pre-op appointment a few days before his surgery. I honestly wondered why I needed to bother getting Rowan out of daycare to take him since all they did was ask me questions.
Surgery day
No food after midnight, no breastmilk for four hours before arrival, and no water for two hours prior to arrival. I’ve heard other providers count breastmilk as a clear liquid, so use your judgment or talk with your doctor.
We had to be at the outpatient surgery center by 6:30 in the morning. It was rough because Rowan usually nurses throughout the early morning hours. Since we have an older daughter we also had to arrange to have her walk to school with a friend.

Give me milk! I know they are still in there!
We filled out various paperwork and were taken back to the pre-op area where we played 20 questions and filled out more paperwork. They gave Rowan a gown and some socks to wear and I had to suit up in the bunny suit that the husbands of c-section moms know all too well. I was allowed to walk him into the operating room.
I sat with him on my lap and held the mask over his face. He was angry. The nurse said if I started inhaling too much of the gas myself to look away. I responded, “but, I could really use a nap.” After a minute he calmed and fell asleep. No IV or intubation, just the gas mask. Much less scary than I had originally envisioned.
They helped me place him on the table and encouraged me to give him a kiss before heading out to the waiting room. He looked so peaceful and tiny!
I joined my husband in the waiting room where there was a screen on the wall with patient numbers and status (pre-op, surgery, post-op). We had a slip of paper with his number on it, so we were able to tell when they actually started the surgery.

The surgery is fast. Maybe 15 minutes. The surgeon came out and gave us the ear drops to put in his ears for five days, some generic post-op instructions, and sent us back to be with him. He was just waking up and he was angry. I mean hulksmash furious. Thrashing. Luckily, we had been warned that this would likely be the case.
I was able to nurse him immediately, though he alternated between screaming and nursing for another 15 minutes or so. Once he was calm and dressed they checked him over once more and we were allowed to take him home.

Drunk baby finally settled down
Our total time from leaving home to returning was just over two hours. My husband and I took the whole day off of work but it turned out that really one of us would have been plenty. That afternoon he was in a fantastic mood. He was back at school the next day.
Recovery
We had to do ear drops for five days, which he hated with a fiery passion. They warned us we might see some discharge during colds. The tubes should fall out on their own after about a year, at which point we will assess if another set is needed.
Time will tell if the tubes will make any large difference, though I have definitely seen slight improvements in his speech. The surgery itself was such a non-issue that I do not have any regrets, either way.
Happy to be home!
Save
